 Approximately 50% of patients develop knee arthritis within their lifespan, so you can imagine why a total knee replacement is such a common procedure. It’s also highly successful – over 90% patients who have undergone a total knee replacement indicate significant pain improvement and improved function is present. According to a patient reported study, change in quality of life assessment per dollar spent ranks in the top three of all major surgical procedures (along with total hip and heart bypass procedures). Currently, there are about 700,000 knee replacements done per year in the United States, and this number continues to increase and may be more than 3 million per year by 2030.
Approximately 50% of patients develop knee arthritis within their lifespan, so you can imagine why a total knee replacement is such a common procedure. It’s also highly successful – over 90% patients who have undergone a total knee replacement indicate significant pain improvement and improved function is present. According to a patient reported study, change in quality of life assessment per dollar spent ranks in the top three of all major surgical procedures (along with total hip and heart bypass procedures). Currently, there are about 700,000 knee replacements done per year in the United States, and this number continues to increase and may be more than 3 million per year by 2030.
Although approximately 95% of patients are much better after surgery, only 80% are fully satisfied. Why? Some patients may have other sources of pain outside the knee joint, while others may have unrealistic expectations – such as believing they will feel like a 20-year old again. 🙂
There are several factors that can affect patient satisfaction rate, such as improved instruments, pain control, anesthesia techniques, therapy, as well as better material and implant design. However, none of these examples reportedly have affected the satisfaction rate even though every other parameter has improved. Examples of improvements include less pain after surgery, better motion, quicker recovery, shorter stay in the hospital, and improved survival of the prosthesis. So, what are we missing?
The modern knee replacement has been around since 1974, and although there have been many implant design changes, the goal has remained the same – place the implants in a way to restore the alignment of the leg, so that a line from the center of the hip to the center of the ankle goes near the center of the knee. Bone cuts are made to accomplish this. Traditionally, rods in the bone are used to reference these angles. The error is up to 3 degrees. More recently, navigation with cameras or accelerometers have improved the accuracy to close to 1 degree.

Once the cuts are made, trial implants are placed and we balance the knee in extension (straight) and in flexion (bent). This means releasing the ligaments to fit the way we made the bone cuts to have equal tension. So, we put everyone’s total knee in the same way and then adjust the soft tissues to fit. But perhaps that is backwards.
We all look different (if not identical twins)…and same goes for our knees. Sometimes the bone is wider, narrower, angled differently – even before the deformities associated with arthritis occur. So, maybe each person’s knee should be placed a little differently. Rather than adjusting the ligaments to fit where we cut the bone, maybe we should make some adjustments to where we put the prosthesis, to follow a patient’s natural ligament tension.
Mako™ Robotic-Arm Assisted Technology
Mako™ Robotic-Arm Assisted Technology allows for precision, and an individualized approach, in knee replacement surgery. Mako uses cameras and arrays attached to the femur (thigh bone) and tibia (shin bone). This allows the robot to know, within less than 1mm and 1 degree of angle, exactly where the knee is in space. A preoperative CT image is obtained and loaded in the computer before surgery.
The robotic arm also guides the surgeon to make the bone cuts to the same degree of accuracy. Instead of cutting the bone first, the surgeon exposes the knee and registers multiple points on the bones to sync the computer CT image to the patient’s knee. Then, before any bone cuts are made, the ligaments are tensioned in different positions. This data is then presented on a computer screen for the surgeon to see.
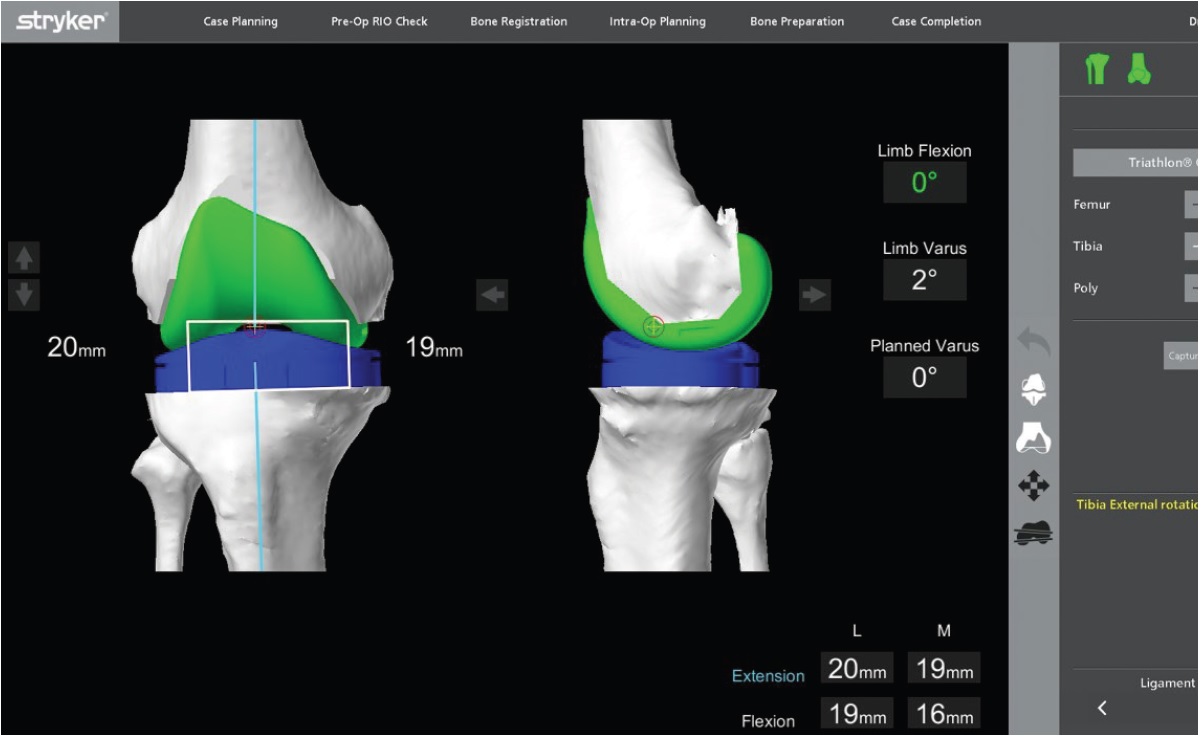
This screen tells the surgeon before any cuts are made, if they are made in this level and angle on the screen, where a knee will be tight or loose as far as ligament balance. Then, the surgeon can change the position of the implants on our screen and see how that affects the knee function. This allows the surgeon to individualize the position of the tibial and femoral component to optimize the knee ligament balance. The robotic arm accuracy then allows the surgeon to duplicate the virtual bone cuts onto the patient’s knee.
This process, unlike a standard knee replacement technique, allows the surgeon to “practice” before any irreversible cut is made. Mako partial knee replacement has shown this technique to produce better outcomes than all other partial knee replacements in several studies. These studies show quicker recovery, better function and better pain scores after recovery. The total knee data is early, but very encouraging. The application was released less than 2 years ago, so no long-term data is yet available.
To learn more about Mako Robotic-Arm Assisted Technology at Central Indiana Orthopedics, visit https://ciocenter.com/services/surgery-revision/

